
Every year, review contractors issue an estimated 2 million requests to healthcare providers for medical documentation and records, according to the Centers for Medicare & Medicaid Services (CMS).
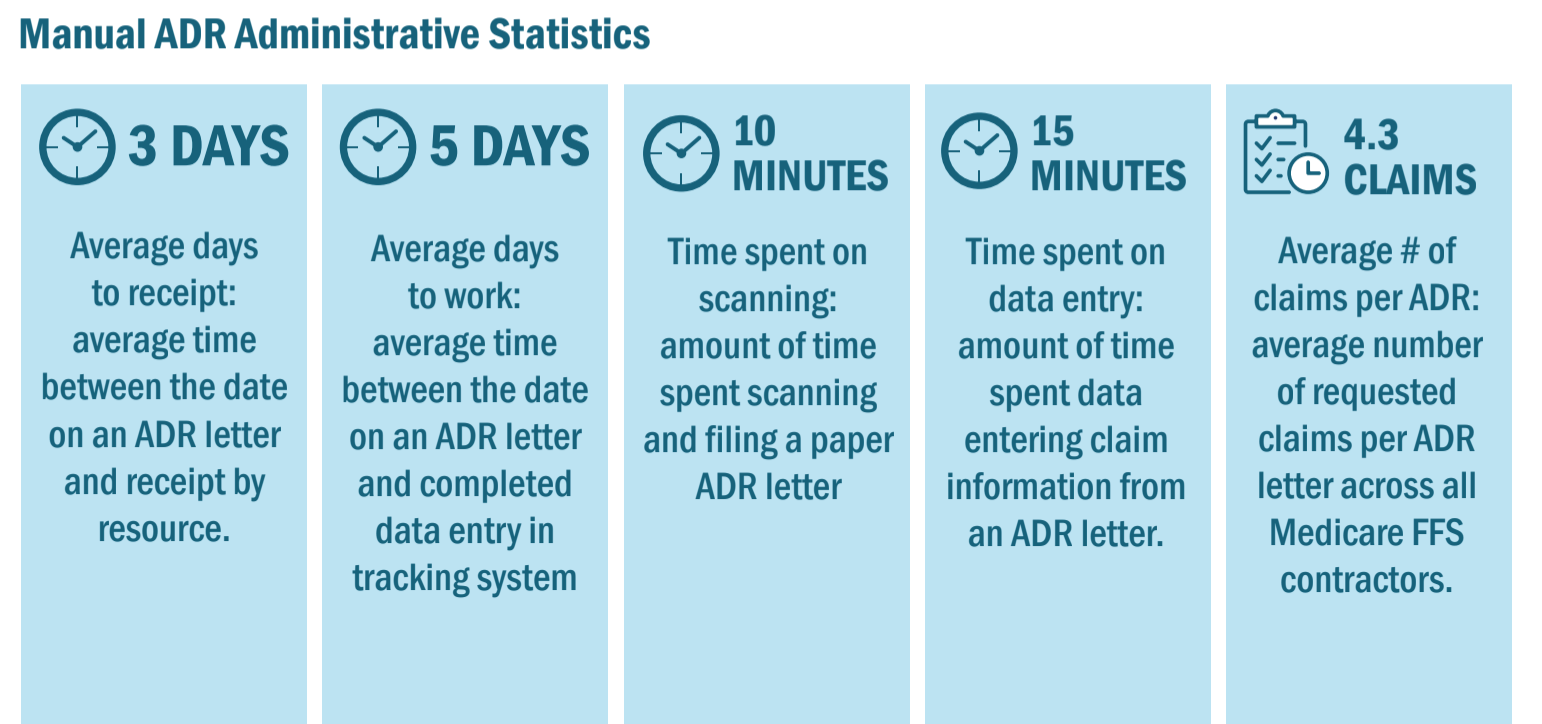
Often, these requests are fulfilled through cumbersome manual processes requiring the review contractor to mail the request for documents, and the provider to print out medical records, compile documentation and submit back to the contractor by mail or fax. The sheer volume of activity reveals workflow gaps and efficiencies in a process that can be up to 90% manual and at risk for data quality issues.
The common sense solution is technology. A comprehensive, integrated audit management system can become the backbone for your audit activity, leading to process improvement, cost savings and reduced labor hours.
But finding an ideal technology-based solution that fits your needs can take a bit of research up front. To help you get started, use this list of five essential features the best audit management systems should offer.
1. Enhanced case management
The first thing a good audit and compliance software should offer, at base, is overall enhanced case management. There are several ways to define “enhanced,” but the most useful tools include status models, intuitive work queues, activity notifications and an electronic repository for documents.
- Status models: All team members should know the progress of an audit response in real time at all times. The system should work in real time to allow for collaboration among previously siloed team members.
- Intuitive work queues: Relevant staff should receive auto-generated, real-time work lists letting them know what they should be working on and when, to avoid any downtime in the audit response process.
- Activity notifications:To further avoid downtime, staff should be notified immediately through the software when they need to begin their role in the audit response process. This also avoids the hassle of communication with physical inter-office memos or flooded inboxes.
- Electronic document repository: The system should consolidate all the various pieces of correspondence and electronic documentation related to the audit in one electronic repository, accessible to all authorized staff.
With these basic features in place, teams can make huge progress in moving from cluttered stacks of medical documentation with manual processes and spreadsheets to more streamlined case management using the right technology.
2. Full automation
The sheer amount of time it takes to complete manual data entry in a hospital setting is cause enough to justify a more high-tech approach to audit management. Teams rely on nurses or financial assistance professionals to complete data entry, preventing staff from working on other worthy projects related to appeals, denials, project management, etc. This also requires significant manual “monitoring” of the billing system because of the high probability of human error.
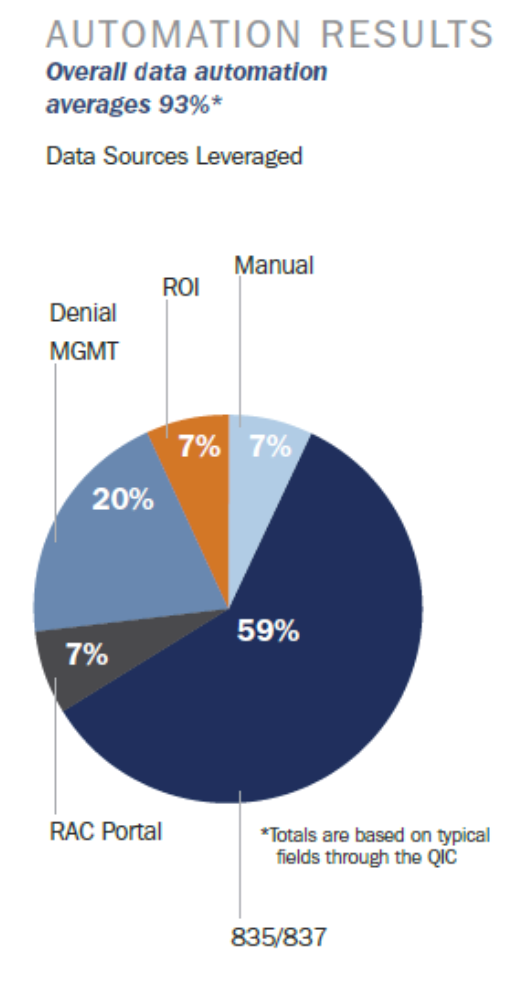
Good audit management software not only automatically enters data, it then uses that data to improve workflows and automate processes. By integrating with HIS systems, audit management systems can pull claims and payment data and use that information to populate required fields in the audit management process. This eliminates manually entering information from the audit, pulling information from claims and remittances and sending claims and communications by hand.
With automated audit management technology, a team can take its process from 90% manual to 93% automated, requiring very little human involvement whatsoever. (The other 7% encompasses things that aren’t data or numbers-driven, like dates verification, notes, etc.)
3. Customizable tools
Not all audits are created equal. Medicare audits are managed by the federal government with one set of rules while Medicaid audits can vary state to state and even between different contractors conducting the audits. Commercial audits can be wildly different depending on the contents of your individual contract with each payer.
That’s why a great audit management software will allow for customization based on the type of audit you’re working with and the requirements within your audit contract. The solution should be configurable to specific audit and denial rules within one single tool to avoid confusion between audit types and to allow for better process optimization within each separate type.
4. Integration and electronic document submission
Every system and vendor used in the audit response process needs to be directly connected, enabling an integrated, streamlined approach; seamless data sharing; and automated workflows. Manual work that requires significant staff time continues to plague existing processes and oftentimes is the result of the audit software not “talking” to other systems.
At minimum, a good software solution should work with esMD to receive and submit audit documentation from CMS. But a great solution should also have the ability to provide custom electronic interfaces with specific commercial payers, provided they are willing to accept electronic documentation.

5. Comprehensive reporting
It’s not just denied dollars that should be tracked and reported on regularly. A great audit management solution provides comprehensive reporting on clearly organized dashboards that can be shared between staff.
The software should allow for integration of outside, applicable systems that show a clear view of at-risk dollars in real time. Accurately reporting on denied dollars, including dollars at-risk vs. dollars that have already been recouped, gives a much clearer picture of the hospital’s overall financial health rather than looking at individual claims.
Aside from monitoring financial health, a good audit management system should also provide real-time access to account status and worker productivity. Knowing how your team is performing at any given point in time is critical to defending process changes and spurring improvement in the long and short term.
Avoiding feature overwhelm
Within these five bullets, there are quite a few features. For a hospital that has relied on manual processes, the idea of investing in a solution that provides all of the above overnight seems overly challenging, sometimes not even worth attempting. Which brings us to our final bonus feature of a great audit management solution: scalability.
When introducing new health information management technologies, ensuring an easy and painless transition for end-users is essential for success. Dividing the project into phases helps. For example, a hospital that currently uses manual processes could spend 6 months adjusting to just the features in points one, two and three: enhanced case management and automation within a customizable interface.
This gives users time to adapt to changes in their everyday work, including notifications, workflows and automated data entry. Once management feels end users are adequately settled in, the team can explore further features, like those in points four and five: integration, electronic document submission and reporting. By this point, the team should have extensive experience in ensuring deadlines, automating processes and measuring and reporting out on success.
Finally, once all features are in place and the team is used to them (a process which could take months to even years), the next phase is process improvement. Now that these features are in place, how can you change and evolve your process to further protect reimbursement dollars?
Freeing up internal resources
Integration and electronic submission is not something that can always be handled entirely by a hospital’s health information management team. Often, the IT department plays a role in setting up new technologies and features.
This explains why some hospitals feel they can never move past phase one and work only within basic features. If IT is already busy with their own projects, how can the two teams coordinate efficiently enough to implement more advanced audit management features?
The answer is not one-size-fits-all. Every hospital is different, with some taking extra effort to get IT on board. However, If IT resources are not available, your platform can still operate on its own and deliver value. That value is further enhanced when fully integrated with your other systems and fitting seamlessly into your broader health information management strategy.
Choosing the right partner

Beyond the technical requirements of a solution, it’s essential the vendor with which you choose to partner understands the complexity of the audit landscape and can facilitate the continued evolution of required processes.
This means finding an expert vendor that has the ability to look ahead, identify potential impacts on the workflows, and proactively make appropriate system enhancements to continue to drive a seamless and efficient audit management process.
If you’re looking for a vendor with these qualities that can provide all the audit management software features in this article and more, look no further than Bluemark’s Blueway Tracker.
Blueway Tracker is a cloud-based audit management platform developed to support Medicare, Medicaid and Commercial Payers audits. It is the most powerful audit management and response solution available in the market today.
Learn more about Blueway Tracker and schedule a free, no-commitment software demonstration today.




