
Patient outreach is the process of establishing a financial relationship with your self-pay patient population. It works to position financial counselors as a resource to help patients with medical expenses the same way nurses, doctors and specialists assist with medical care. At the very least, outreach involves getting patient contact information and permission to contact them in the future regarding their medical payments.
The goal of patient outreach is to make contact with a patient as early as possible to facilitate future communication regarding the patient’s account. The process must be done efficiently, but with immense tact for best results in establishing strong relationships. Each hospital or health system has established procedures and etiquette for outreach, but as with every process, there’s always room for a little improvement!
Why is patient outreach important?
Building a relationship with your self-pay patient population is a key principle of success in healthcare finance. There are many misconceptions around medical financial assistance, and outreach can help demystify the process by educating patients.
One such misconception is the potentially negative stigma around Medicaid and charity care as a welfare program in the eyes of many patients. The Affordable Care Act attempted to destigmatize healthcare assistance programs by redefining programs like Medicaid as simply a subsidized program that covers medical costs for individuals and families. Outreach education continues with this repositioning by showing patients that Medicaid is simply a subsidized program based upon your family circumstances at the time of care.
Another misconception is that financial counseling is closely associated or overlapped with the collections department. Patients often falsely believe that anyone who contacts them in regard to medical payments is seeking to collect money. While hospitals may have financial counselors involved in collecting deductibles and copays, collections is generally not a task charged to the financial assistance department.
Finally, this is not necessarily a misconception, but another aspect of financial assistance patients don’t often realize and may need educated on is that financial assistance is a win for both the hospital and the patient. The hospital’s expenses are covered, as are the patients. Additionally, when one family member is enrolled in Medicaid, their entire family is typically enrolled and they may be eligible for coverage on future visits.
When is the best time to reach out to patients?
There are two times to reach out to patients: Either when they are still on hospital grounds or once they’ve gone home. Both circumstances require different outreach methods.
• Outreach while on hospital grounds
Ideally, patients should be approached for financial assistance enrollment as early as possible. However, there are certain sensitivities around the logistics of approaching a patient’s bedside which must be considered when initiating the relationship.
To ensure your staff speaks to the patient without being insensitive, you may want to make financial assistance part of the discharge checklist. If a patient is set to leave, either assign a staff member to check in with them and start the enrollment process, or ask the patient to check in with the financial counseling office prior to leaving.
• Outreach from home
If you are unable to reach out to a patient while they are still in the hospital, you must move on to option two and attempt to contact them at home. This option is less ideal as you may be confused for collections or your outreach attempts ignored more easily than if you were at their bedside. But it is not impossible to establish a relationship after the patient’s hospital visit.
There are two types of outreach at this point: direct and passive. Direct outreach is proactive and involves calling patients over the phone to engage them in the financial assistance enrollment process. Direct outreach works well for getting a patient’s attention, but can be costly and time consuming. It is best to focus on high-dollar accounts first when making phone calls for outreach.
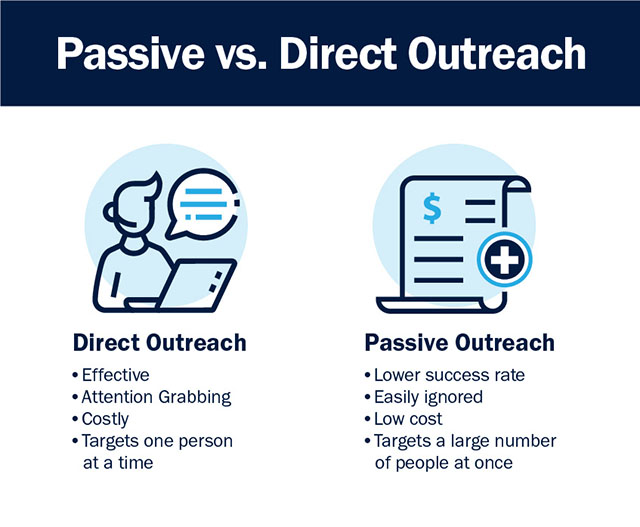
The second type of outreach is passive, which involves including information on medical bills or other correspondence directing the patient to the financial assistance office for help covering their payments. In this case, impetus is on the patient to reach out, not your staff. This method is not as effective and can be easily ignored, but it does allow you to target a larger number of accounts at once.
What are some best practices for patient outreach?
Outreach is a nuanced process that tends to be highly specific to the hospital or health system in which it takes place. However, there are several key best practices that can be followed universally.
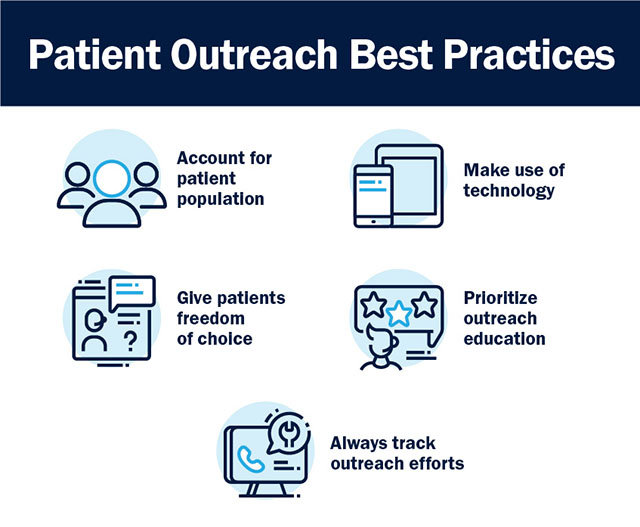
1. Account for your patient population’s evolving demographics.
Part of the population is still comfortable answering the phone or responding to persistent (not annoying!) voicemail messages. That part of the population tends to be older, and only makes up a portion of patients today.
Younger generations tend to prefer self-service tools that allow them to engage in the financial assistance process on their terms, when they want and in their desired communications channel. Instead of operating only through phone calls, branch out into using emails and texts in your outreach process to keep up with evolving demographics.
2. Make use of technology.
Even if the majority of your patient population is older or has been responding fairly well to phone calls for years, you may be able to capture and engage several other patients through emails and texts.
Technology doesn’t just give you the means to send email and text communication. It also:
- Facilitates the use of electronic tools like program screening microapps
- Allows for self-service portals that can initiate the engagement process more effectively
- Automates workflows for increased time management
- Increases security for sensitive information communicated electronically.
Some processes have been done by hand for so long you may no longer notice. If snail mail, phone calls and manual spreadsheets are just the way you’ve always done it, it doesn’t hurt to take a peek behind the curtain and explore the possibility of a tech upgrade in your outreach process.
3. Give patients freedom of choice.
Once you’ve found the channel in which a patient is most comfortable engaging with, let them choose how they wish to communicate after first contact. Provide 2-4 options and points of access and make note of which one they specify is best for connecting. From there, you can also ask which times of day they prefer to be contacted.
Not only does this increase the likelihood of regular patient response, it puts them behind the driver’s seat and gives them some control over the situation. Freedom of choice is an underused tactic for patient cooperation that can set a solid foundation for the future of the relationship.
4. Prioritize education in your outreach.
This one is huge. Patients must understand the role you’re playing is to help them, not send them to collections or ask for money. Be aware of phrasing, and know what conversation openers tend to elicit a positive response from patients. Then, train your employees on what words and phrases work and don’t work.
The goal is to provide education without coming off as insincere or giving the patient a reason to cut off contact before the relationship is even established.
5. Always track outreach efforts.
Remember, a huge part of financial assistance write-offs are dependent upon demonstrating effective, proactive outreach activity. The best way to do this is to use a software or other electronic system that can track your team’s efforts and ensure they are compliant with your internal rules as well as external tax regulations.
Many hospitals underestimate the value of tracking outreach internally, but this data is invaluable. Knowing how often people in different age groups respond to certain outreach efforts can help manage your staff’s time and better segment calling lists. You can also track metrics to help determine the best times to call and how to open the conversation. When it comes to outreach, hard data is the best teacher.
Technology to improve patient outreach
Take your patient outreach process online with the MAPS-clear patient portal. This standalone portal works as a web-based application that supports proactive patient outreach activities, remote financial counseling, and new contactless engagement initiatives.




